News Update
Study: Large Accountable Care Organizations Committed to Overhauled Medicare Program
While most Accountable Care Organizations (ACOs) have committed to continue participating in the recently overhauled flagship Medicare Shared Savings Program (MSSP), physician-led ACOS are leaving at a higher rate than in 2017, new research from the Duke-Margolis Center for Health Policy and Leavitt Partners shows.
Highlights of this research appear in a Health Affairs Blog posted this week.
The most recent tracking showed that more than 1,000 public and private ACOs provide health care coverage to approximately 33 million Americans. In 2018, more than half of these ACOs participated in the Centers for Medicare & Medicaid Services (CMS) MSSP program.
Late last year however, CMS released its Pathways to Success rule, overhauling MSSP, its largest ACO program. The new 2019 MSSP participant list showed that 74 ACOs dropped out of MSSP at the end of 2018, representing 13 percent of participating ACOs.
Duke-Margolis and Leavitt researchers examined this data to determine the early impact of the new rule, and found:
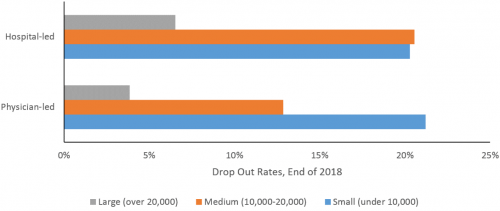
- Hospital-led ACOs, which tend to be large, as well as large ACOs of any type, had lower dropout rates at the end of 2018. This early look at new dropouts from the MSSP program suggest the rule is not driving large ACOs out of the program, but rather that they are willingto accept increasing risk for the cost of the care they provide, also known as downside risk.
- Overall, the ACO dropout rate increased modestly at the end of 2018, in contrast to the two previous years when it decreased.
- As part of its overhaul of MSSP, CMS assigned different downside risk requirements for high-revenue and low-revenue ACOs to reflect their different capacity to bear risk, and to encourage more small and physician-led ACOs to participate in the program. So far, revenue status does not appear to be consistently correlated with ACO dropout rates, and is not highly correlated with ACO size or physician ownership.
- Physician-led ACOs, which tend to be smaller, had higher dropout rates than hospital-led ACOs, despite new policies to support low-revenue ACO. Small physician-led ACOs had the highest dropout rate at the end of 2018, so how well “low revenue” status supports these particular types of ACOs bears close watching.
“If the ACOs leaving were not likely to succeed, or were not seriously engaged in changing care delivery to improve value, then lower participation is not a bad outcome,” said Mark McClellan, MD, PhD, director of the Duke-Margolis Center. “If organizations that were likely to succeed are exiting, especially smaller physician-led organizations that have had promising results to date, then further policy adjustments may be needed.”
“The significant changes to MSSP are a likely reason why ACOs decided to leave, suggesting there may be more departures as current contracts expire over the next two years,” said David Muhlestein, PhD, JD, chief research officer at Leavitt Partners. “However, we find little evidence that increased risk facing large ACOs, whether hospital- or physician-led, has deterred their continuation in the program.”
About Leavitt Partners
Leavitt Partners is a health care intelligence business. The firm helps clients successfully navigate the evolving role of value in health care by informing, advising, and convening industry leaders on value market analytics, alternative payment models, federal strategies, insurance market insights, and alliances. Through its family of businesses, the firm provides investment support, data and analytics, member-based alliances, and direct services to clients to support decision-making strategies in the value economy. For more information please visit www.LeavittPartners.com.
