Implications of Global Experiences with Accountable Care
This project aims to address these challenges by accelerating the uptake of successful policy, payment, and delivery innovations from abroad that can improve the care of high-need, high-cost populations in the US. Our team will identify globally proven solutions that can be integrated with emerging local, state, and national payment facing US healthcare institutions. We will use these findings to demonstrate how organizations can draw on global experiences to create a combination of innovations that can succeed under new payment models to help address currently unmet challenges to providing integrated, comprehensive care to high-need, high-cost patients.
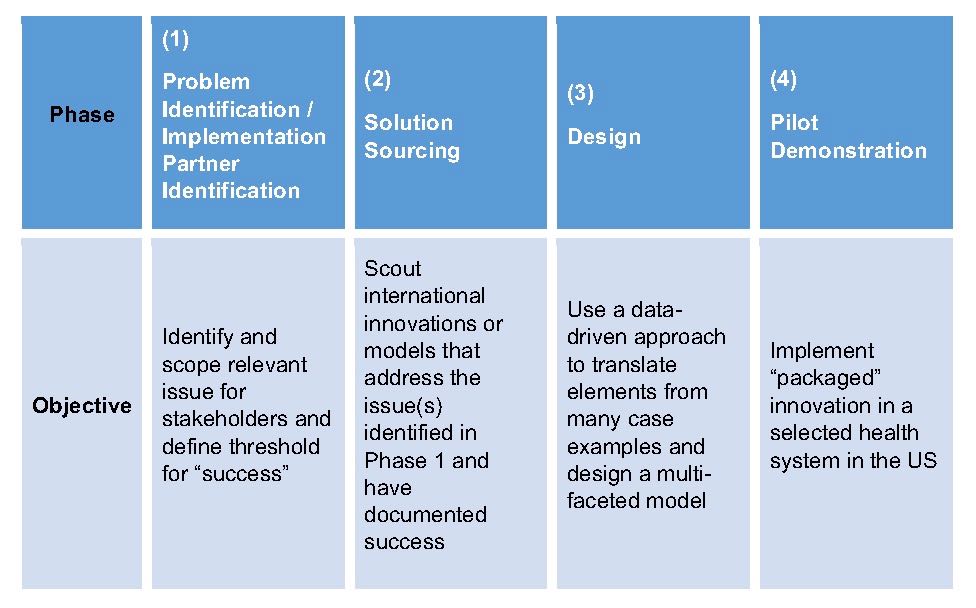
This work is currently at the end of Phase 1 and beginning of Phase 2, identifying international innovations or models that address the identified challenges. Below is a table showing the outlined phases for this project:
This project builds upon previous work regarding the implications of global experiences with accountable care for the United States' healthcare system with the aim of accelerating uptake of successful experiences with accountable care and other innovations in the US by promoting the exchange of best practices and knowledge. Based on prior work supported by the Commonwealth Fund, the Duke-Margolis team is identifying practical lessons that can be adopted by a wide range of policy makers and payers in the US to accelerate health care reform domestically. Recently, the team was awarded a follow-on project to accelerate the uptake of successful policy, payment, and delivery innovations from abroad and identify US healthcare systems and/or communities to implement major components of or full integrated delivery and payment reforms.
The project case studies on lessons learned, released January 30, 2017 at a public event, “Translating International Models of Care for High-Need, High-Cost Populations in the United States” as well as the associated research articles:
Research Papers:
Accountable Care Reforms Improve Women's And Children's Health In Nepal
Case Studies:
Case Study: Better Together (United Kingdom)
Case Study: Zio Integrated Care Network (the Netherlands)
Case Study: Gesundes Kinzigtal (Germany)
Previous Case Studies:
Spain: Reinventing Chronic Care Management for the Elderly (Ribera Salud Hospital System)
India: Enhancing Care Management for Diabetes Patients in Rural Communities (SugaVazhvu Healthcare)
Mexico: Preventing Chronic Disease Through Innovative Primary Care Models (Casalud)
Research Team
Mark McClellan, MD, PhD
Director, Duke-Margolis
Andrea Thoumi, MPP, MSc
Managing Associate
Krishna Udayakumar, MD, MBA
Founding Faculty, Duke-Margolis
Associate Professor of the Practice of Global Health, Duke Global Health Institute
Associate Professor - Track IV in Medicine, General Internal Medicine
Jonathan Gonzalez-Smith, MPAff
Senior Research Assistant
Alexander Gunn, MBS
Research Assistant
Nicole Davis
Program Intern, Innovations in Healthcare
Kushal Kadakia
Undergraduate Research Assistant
Advisory Group
2017-2018
William Conway, CEO, Henry Ford Medical Group
Molly Coye, Executive in Residence, AVIA
Victor Dzau, President, National Academy of Medicine
Don Goldmann, Chief Medical and Scientific Officer, Institute for Healthcare Improvement
Mark Humowiecki, General Counsel and Senior Director, Camden Coalition
Ann Lewis, CEO, CareSouth Carolina
Brian Marcotte, President and CEO, National Business Group on Health
Jose Peña, CEO, CMO, Rio Grande Valley ACO
Jonathan Perlin, President, Hospital Corporation of America
Mai Pham, Vice President, Anthem
David Pryor, Executive Vice President, Ascension
Dave Richard, Deputy Secretary for Medical Assistance, North Carolina DHHS
Iyah Romm, Care CEO, Sidewalk Labs
Lew Sandy, Senior Vice President, UnitedHealth Group
Deidra Singleton, Acting Director, South Carolina Department of Health and Human Services
Ross Wilson, Chief Medical Officer, New York Health and Hospitals Corporation
2016-2017
Jeffrey Brenner, Medical Director, Urban Health Institute and Executive Director, Camden Coalition
William Conway, CEO, Henry Ford Medical Group and Executive Vice President, Henry Ford Health System
Molly J. Coye, Social Entrepreneur in Residence, Network for Excellence in Health Innovation
Victor J. Dzau, President, National Academy of Medicine and Vice Chair, National Research Council
Palmer “Pal” Evans, Executive-in-Residence, Management Innovations in Health Care, Eller College of Management, the University of Arizona
Robert Galvin, Chief Executive Officer, Equity Healthcare
Don Goldmann, Chief Medical and Scientific Officer, Institute for Healthcare Improvement
Ann Lewis, Chief Executive Officer, CareSouth Carolina
David Morales, Executive Vice President and Chief Strategy Officer, Steward Health Care System
Stephen Ondra, Senior Vice President and Enterprise Chief Medical Officer, Health Care Service Corporation
Bela Patel, Assistant Dean of Healthcare Quality and Division Director for Critical Care Medicine, University of Texas Health Science Center in Houston
Jose Peña, CEO and Chief Medical Director, Rio Grande Valley Accountable Care Organization
Jonathan B. Perlin, President, Clinical Services and Chief Medical Officer, Hospital Corporation of America
Hoangmai Pham, Chief Innovation Officer and Acting Director of the Policy and Programs Group, Center for Medicare & Medicaid Innovation
David B. Pryor, Executive Vice President and Chief Clinical Officer, Ascension
Steven M. Safyer, President, Chief Executive Officer, Montefiore Medicine
Lewis G. Sandy, Senior Vice President of Clinical Advancement, UnitedHealth Group
Ross Wilson, Senior Vice President of Quality, Corporate Chief Medical Officer, and a Corporate Officer, NYC Health + Hospitals
Funding
This project is funded by The Commonwealth Fund. The views expressed in written conference materials or publications and by speakers and moderators do not necessarily reflect the official policies of the Commonwealth Fund.