Integrated Pain Management: Lessons from North Carolina Health Systems and Beyond
Project Overview
In North Carolina, deaths due to medication/drug overdoses have been steadily increasing since 1999, and the vast majority (90%) of these are unintentional. Many of the current approaches for combating the opioid crisis are reactive, such as prescription drug monitoring programs and prescribing guidelines for opioids. These efforts have resulted in lower opioid prescribing rates, but do not address the underlying problem of untreated pain. In the absence of appropriate pain relief and meaningful access to non-opioid alternatives, there is rising concern that these efforts are resulting in barriers to appropriate pain management and adverse consequences (e.g., overdose or suicide) for patients currently dependent on opioids.
Integrated pain management models, with pharmacologic/drug therapies, psychological/behavioral care, physical therapy, occupational therapy, and other services, can effectively address the burden of pain. While there is evidence for the effectiveness of these approaches, expanding the use of such models requires identifying best practices for implementation.
As part of a broader portfolio of projects to reduce the harms of opioids in North Carolina, the Duke Department of Orthopaedic Surgery and the Duke-Margolis Center for Health Policy are launching an effort to understand better how integrated pain management models are being developed and implemented in health systems, and to identify how such models can be deployed more broadly throughout the state. Integrated pain management engages psychological/behavioral care, physical therapy, occupational therapy, and other services in addition to pain management prescription drugs. By focusing on and working to resolve untreated pain, integrated pain management approaches hold promise to provide lasting relief to patients while minimizing or eliminating the use of opioids.
This initiative aims to:
-
Identify integrated pain management models that improve outcomes and reduce opioid-related risks,
-
Describe organizations that have successfully undertaken this approach, and
-
Recommend how better to implement these models in North Carolina and similar states.
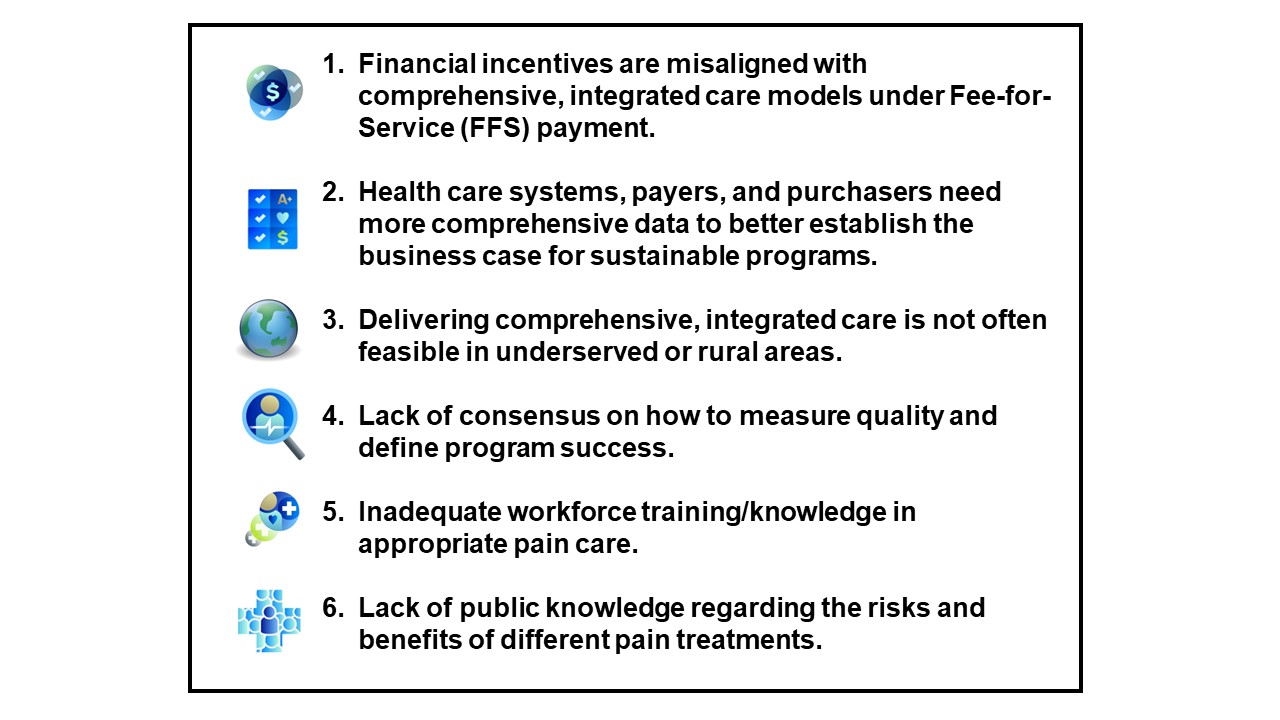
Challenges Surrounding the Implementation of IPM
To better understand the challenges surrounding implementation of IPM programs, the Duke-Margolis Center for Health Policy and the Duke Department of Orthopaedic Surgery held a roundtable in February 2020 with more than 30 stakeholders including payers, purchasers, employers, health policy experts, pain researchers, front-line clinicians, and patient representatives. Discussions focused on key challenges associated with the development, implementation and maintenance of IPM programs. We highlight the most important takeaways from that meeting below.
Funding
This project is part of the Duke School of Medicine Opioid Program portfolio, a grant funded by the Duke Endowment and administered through the Duke Department of Population Health Sciences. The Opioid Program portfolio projects are designed to save lives and reduce the harmful impact of opioids in North Carolina through the development, implementation, and/or evaluation of sustainable, system-level interventions.
Research Team

Trevor Lentz, PhD
Assistant Professor in Orthopaedic Surgery
Margolis Core Faculty

Robert Saunders, PhD
Senior Research Director, Health Care Transformation
Adjunct Associate Professor
Executive Team Member
Margolis Core Faculty

Katie Huber, MPH
Policy Research Associate

Christine Goertz, DC, PhD
Professor of Orthopaedic Surgery
Margolis Core Faculty
